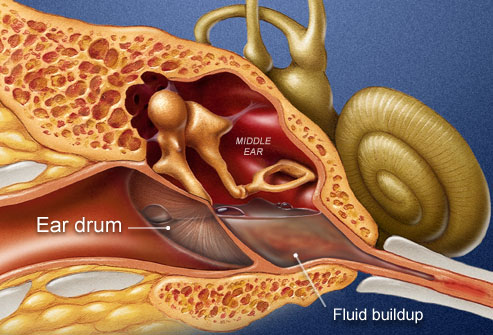
Ear infections in your child. The ENT Center of Austin can help with the recovery. In most cases it will run its course. No treatment may be necessary other than relieving the pain with some OTC medicines. If it reoccurs on a regular basis, this is a sign that we’ll need to step-up our resources to rid that kid of repeat performance.
Just recently, another weapon has been discovered that doesn’t involve what we have been using as treatment for years. While it has yet to enter the marketplace of practice, it gives hope for those who suffer from a long-term rash of middle ear infections.
Turns out, it’s a pretty unique approach.
The DNA Fix
We’re going to swim over to our favorite resource — the online periodical “Science Daily.” About a year ago, to be exact October 2012, they published this stunning concept from a team in the Research Institute at Nationwide Children’s Hospital. Turns out the researchers started to drill deeply into how an immune defense protein that’s usually found in the middle ear relates to a community of bacteria in that part of the body.
Our source reports:
“The bacterium nontypeable Haemophilus influenzae (NTHI) causes a wide range of diseases of both the lower and upper airways, including middle ear infection. NTHI, like most other bacteria, can form a biofilm, a robust community of bacteria that allows the bacteria to evade the host’s immune system and protects the bacteria from antibiotics and other therapies designed to kill them.”
“Human beta-defensin-3 is an antimicrobial defense protein expressed in the middle ear of humans and other mammals that kills both Gram-positive and Gram-negative bacteria. Previous research has shown that if expression of beta-defensin is disrupted, the host’s ability to control the bacteria in the upper airway is altered and infection worsens.”
“Investigators in The Research Institute at Nationwide Children’s Hospital hypothesized that human beta-defensin-3 might lose its power to kill NTHI if it got caught up within the extracellular DNA that makes up a biofilm’s outer layer, thus preventing its contact with bacteria within the biofilm.”
Pretty heady stuff, eh? We’ll boil it down for you.
In Other Words
What the article is basically saying is that by attaching a certain type of protein to the bacteria, it ruins the day for that junk called biofilm in the ear canal.
“Similar to other microorganisms, NTHI can create a strong colony of bacteria, known as a biofilm. This permits the bacteria to avoid the person’s immune system, while keeping safe from antibiotics and other treatments that try to destroy them.”
“Lauren O. Bakaletz, Ph.D., director of the Center for Microbial Pathogenesis, explained:”
“Antimicrobial host defense proteins, like human beta-defensin-3, have been shown to bind to non-host DNA. This interaction has an impact on the defense protein’s ability to function.”
“The ability to restore antimicrobial defense protein activity is encouraging, since biofilms are resistant to most treatments, including traditional antibiotics,” Dr. Bakaletz said.”
With this new knowledge, other scientists will be able to manufacture unique treatments. As Dr. Bakaletz concludes, “This approach would likely bolster the ability of the innate immune system to manage NTHI-induced biofilms, avoiding the need for antibiotics or empowering the use of antibiotics we already have in our arsenal. Doing so could help diminish the recurrent nature of middle ear infection.”
Image Source: earinfectionzone.com/wp-content/uploads/2013/05/Ear-Infection-Remedies.jpg

